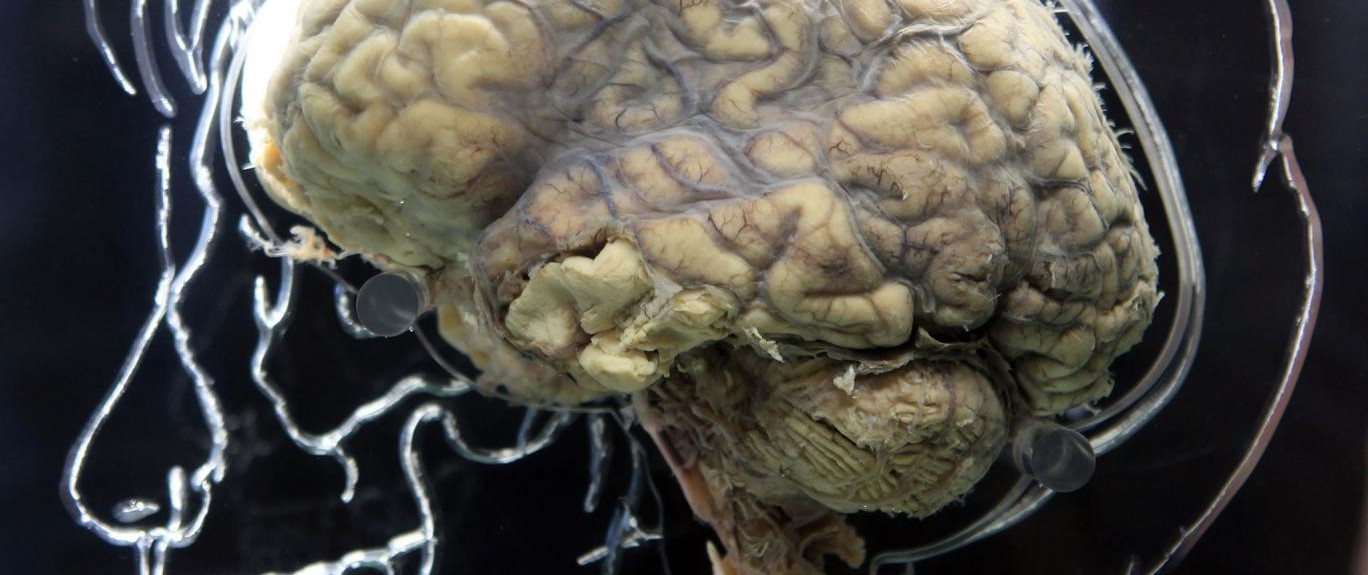
A Johns Hopkins University study found that combat veterans are not seeking out treatment for their brain injuries or mental trauma until the problem becomes too big to ignore. Waiting for a “wake up call” before confronting the problem leaves vets more at risk for depression, insomnia, memory issues and suicide.
It seems like common sense to wait for a health problem to clear up on its own before seeking out a doctor. Medical bills are expensive, and appointments are tough to keep for vets who must travel to the nearest VA hospital. While this might work for small ailments like a twisted ankle or stomach ache, allowing brain injuries to fester untreated and undiagnosed can have disastrous consequences.
As the study put it, veterans who don’t nip their brain injuries in the bud early are abruptly “thrown into a canyon” of despair and cognitive struggles.
Researchers interviewed 38 Army combat veterans in 2013 and 2014 and quickly found a pattern. Veterans were prone to play down their injuries and become distant from their loved ones. They remained unwilling to admit that their mental health was deteriorating until a “wake up call” like a panic attack or breakdown forced them to acknowledge the problem.
Veterans with spouses and families tended to fare better because they had someone to push them to get treatment. Those who lived closeby a VA hospital also tended to do well because they had more access.
Study author Rachel P. Chase said part of the problem is that combat veterans hide their invisible injuries in order to remain in the service.
The bigger problem is the “no, not, never code” that GIs adopt to deny exposure to blasts because they don’t want to abandon their buddies in the fight and the bureaucratic red tape that continues to ensnare combat veterans who often display symptoms that could apply not just to traumatic brain injury, or TBI, but other invisible wounds of war, such as post-traumatic stress disorder, according to Chase.
“One of the vets in the study told us what it was like,” she said. “You go to one clinic, and they tell you, ‘Oh, that’s TBI.’ Then you go to another clinic, and they say, ‘No, that’s PTSD.’ Back and forth and you’re still untreated.”